Introduction
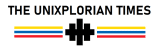
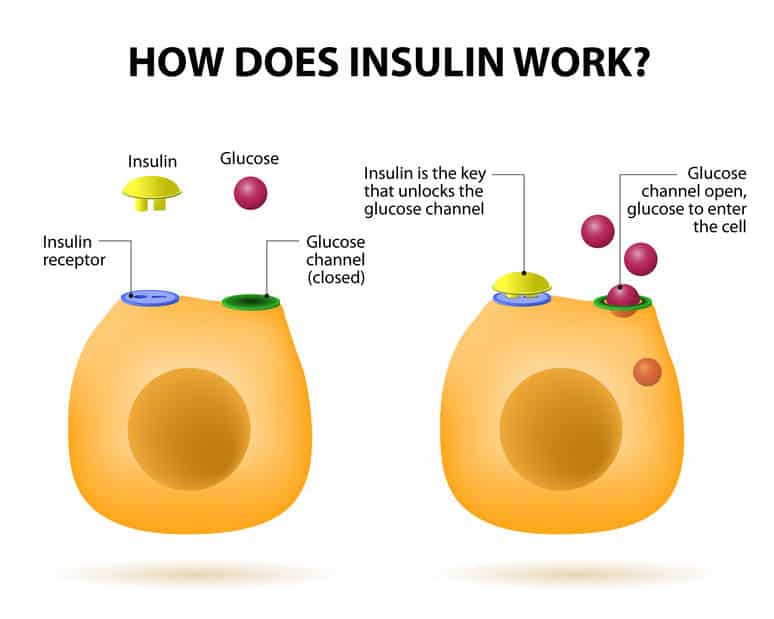
If you have type 1 diabetes, your pancreas doesn’t make or make very little insulin. Insulin helps blood sugar enter your body’s cells for energy use. Without insulin, blood sugar can’t get into cells and builds up in the bloodstream. High blood sugar damages the body and causes many of the symptoms and complications of diabetes.

Type 1 diabetes was once called insulin-dependent or juvenile diabetes. It usually develops in children, teens, and young adults but can happen at any age. Type 1 diabetes is less common than type 2—about 5-10% of people with diabetes have type 1. Currently, no one knows how to prevent type 1 diabetes, but it can be treated successfully by:
- Following your doctor’s recommendations for living a healthy lifestyle.
- Managing your blood sugar.
- Getting regular health checkups.
- Getting diabetes self-management education and support.
What Causes Type 1 Diabetes?
Type 1 diabetes is thought to be caused by an autoimmune reaction (the body attacks itself by mistake). This reaction destroys the cells in the pancreas that make insulin, called beta cells. This process can go on for months or years before any symptoms appear.
Some people have specific genes (traits passed on from parent to child) that make them more likely to develop type 1 diabetes. However, many of them won’t go on to have type 1 diabetes even if they have the genes. A trigger in the environment, such as a virus, may also play a part in developing type 1 diabetes. Diet and lifestyle habits don’t cause type 1 diabetes.
Symptoms and Risk Factors
It can take months or years before symptoms of type 1 diabetes are noticed. Type 1 diabetes symptoms can develop in just a few weeks or months. Once symptoms appear, they can be severe.
Some type 1 diabetes symptoms are similar to symptoms of other health conditions. Don’t guess! If you think you could have type 1 diabetes, see your doctor to get your blood sugar tested. Untreated diabetes can lead to severe—even fatal—health problems.
Risk factors for type 1 diabetes are not as straightforward as prediabetes and type 2 diabetes. However, studies show that family history plays a part.
Testing for Type 1 Diabetes
A simple blood test will let you know if you have diabetes. If you were tested at a health fair or pharmacy, follow up at a clinic or doctor’s office. That way, you’ll be sure the results are accurate.

If your doctor thinks you have type 1 diabetes, your blood may also be tested for autoantibodies. These substances indicate your body is attacking itself and are often found with type 1 diabetes but not type 2. You may have your urine tested for ketones too. Ketones are produced when your body burns fat for energy. Having ketones in your urine indicates you have type 1 diabetes instead of type 2.
Managing Diabetes
Unlike many health conditions, diabetes is managed primarily by you, with support from your healthcare team:
- Primary care doctor
- Foot doctor
- Dentist
- Eye doctor
- Registered dietitian nutritionist
- Diabetes educator
- Pharmacist
Also, ask your family, teachers, and other important people for help and support. Managing diabetes can be challenging, but everything you do to improve your health is worth it!
If you have type 1 diabetes, you must take insulin shots (or wear an insulin pump) daily. Insulin is needed to manage your blood sugar levels and give your body energy. You can’t take insulin as a pill. That’s because the acid in your stomach would destroy it before it could get into your bloodstream. Your doctor will work with you to determine the most effective type and dosage of insulin for you.

You’ll also need to do regular blood sugar checks. Ask your doctor how often you should check it and what your target blood sugar levels should be. Keeping your blood sugar levels as close to target as possible will help you prevent or delay diabetes-related complications.
Stress is a part of life, but it can make managing diabetes harder. Managing your blood sugar levels and daily diabetes care can be more challenging. Regular physical activity, getting enough sleep, and relaxing exercises can help. Talk to your doctor and diabetes educator about these and other ways you can manage stress.
Healthy lifestyle habits are essential too:
- Making healthy food choices
- Being physically active
- Controlling your blood pressure
- Controlling your cholesterol
Make regular appointments with your healthcare team. They’ll help you stay on track with your treatment plan and offer new ideas and strategies if needed.
Hypoglycemia and Diabetic Ketoacidosis
These two conditions are common complications of diabetes, and you’ll need to know how to handle them. Meet with your doctor for step-by-step instructions. You may want to bring a family member to the appointment so they learn the steps too.
Hypoglycemia (low blood sugar) can happen quickly and needs to be treated promptly. It’s most often caused by:
- Too much insulin.
- Waiting too long for a meal or snack.
- Not eating enough.
- Getting extra physical activity.
Talk to your doctor if you have low blood sugar several times weekly. Your treatment plan may need to be changed.

Diabetic ketoacidosis (DKA) is a severe complication of diabetes that can be life-threatening. DKA develops when you don’t have enough insulin to let blood sugar into your cells. Very high blood sugar and low insulin levels lead to DKA. The two most common causes are illness and missing insulin shots. Talk with your doctor and make sure you understand how to prevent and treat DKA.
Get Diabetes Education
Meeting with a diabetes educator is a great way to get support and guidance, including how to:
- Develop and stick to a healthy eating and activity plan
- Test your blood sugar and keep a record of the results
- Recognize the signs of high or low blood sugar and what to do about it
- Give yourself insulin by syringe, pen, or pump
- Monitor your feet, skin, and eyes to catch problems early
- Buy diabetes supplies and store them properly
- Manage stress and deal with daily diabetes care
The Signs and Symptoms of Diabetes Type 1
Are you worried that you, your child, or someone you know may have diabetes? Having some diabetes symptoms doesn’t mean you have the condition, but you should always contact your GP to make sure.
Diabetes symptoms
- Toilet – going for a wee a lot, especially at night.
- Thirsty – being thirsty.
- Tired – feeling more tired than usual.
- Thinner – losing weight without trying to.
- Genital itching or thrush.
- Cuts and wounds take longer to heal.
- Blurred eyesight
- Increased hunger.
These symptoms can affect anyone – adult or child. But some are more commonly experienced by people with type 1 diabetes and can come on quickly.
What are the most common symptoms?
No individual is the same. You may also experience other symptoms, which may not precisely match that of another person and may not be on the list above. However, the most common symptoms experienced by many people with diabetes are increased thirst, going for a wee a lot, feeling tired, and losing weight.

You’re showing diabetes symptoms: what next?
If you feel unwell or your symptoms have come on, quickly seek an urgent appointment with your GP. If you have any diabetes symptoms, you must contact your GP and ask for a blood test for diabetes. Find out more about getting tested for diabetes.
What causes these symptoms?
Diabetes symptoms occur because some or all of the glucose stays in the blood and isn’t used as energy fuel. The body tries to reduce blood glucose levels by flushing the excess glucose in the urine, making you thirsty. High glucose levels passed in the urine are a perfect breeding ground for the fungal infection which causes thrush. But not everyone gets symptoms. 6 out of 10 people have no symptoms when diagnosed with type 2 diabetes.
When to speak to a doctor
You should contact your local GP if:
- You or your child is showing diabetes symptoms
- You believe you or your child is at high risk of developing diabetes
- If you think your partner or a friend is also at risk of diabetes, speak to them and encourage them to seek professional advice.
Diabetes risk factors
Some people are at a higher risk of developing diabetes than others. Depending on the type of diabetes, this can be due to their ethnicity, genetics, or lifestyle choices. These are known as the risk factors of diabetes. Knowing the risk factors and their effects can help you decide if you need to do something to reduce your risk.
Know Your Risk
It’s essential to know your risk of developing diabetes, as it can inform your future decisions. Check your risk of type 2 diabetes using our free Know Your Risk tool – it only takes two minutes. If your score is a moderate or high risk, you’ll need to ask your GP for a blood test.

If you ignore the signs of diabetes
It’s hard to ignore the signs of type 1 diabetes because symptoms can often appear quite quickly. But leaving it untreated can lead to serious health problems, including diabetic ketoacidosis, which can result in a potentially fatal coma.
Although most people with type 1 diabetes are diagnosed in childhood and early adulthood, the symptoms are the same at any age. Adults with type 1 diabetes may not recognize their diabetes symptoms as quickly as children, which could delay their diagnosis and treatment.